Feeling separate is difficult. Many of us have encountered some level of isolation over the last year. Exclusion from communication too can exacerbate our feelings of loneliness, isolation, and frustration. This is felt among people with hearing loss every day [1]. Indeed, as we get older and are more likely to have hearing loss, hospitals and other healthcare services become increasingly essential. So, what happens when a hard of hearing person needs to go to a hospital?
This paper outlines some of the problems that people with hearing loss face in hospitals and why it is essential to reflect on how we might improve the experience. It also outlines how other organisations have taken steps towards a solution.
What is hearing loss?
466 million people worldwide have disabling hearing loss. This is more than 5% of the global population and it is expected to rise to over 900 million (which means one in every ten people) by 2050, thanks to an ageing population and an increasing number of people exposed to dangerously loud noise. Hearing loss is also caused by complications at birth, some infectious diseases, or the use of some drugs [1].
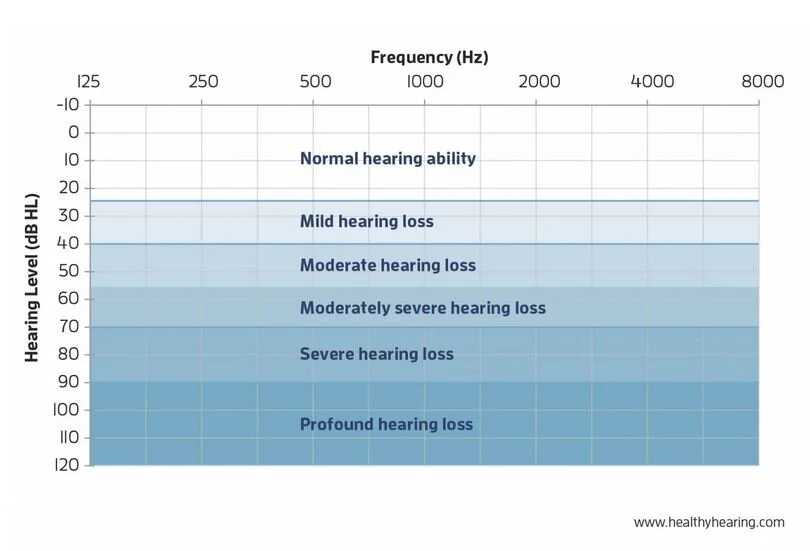
Hearing loss can be permanent or temporary and is measured as loudness versus pitch of sounds. The frequency describes how high the sound's pitch is and is measured in hertz (Hz). The loudness is usually measured in decibels (dB).
The following list shows examples of the volume of familiar noises [2]:
- Breathing: 10dB
- Normal conversation: 40-60 dB
- Lawnmower: 90dB
- Rock concert: 120 dB
- Gunshot: 140 dB [5]
Hearing loss ranges from mild to profound, as shown in the picture below.
Try being hard of hearing for yourself
Can you imagine how the world sounds for a hard of hearing person? Try out this hearing simulator. Click on a sound at its 'normal level', and then try out the different types of hearing loss. The tinnitus example was particularly confronting. The simulation helps those with normal hearing experience hearing loss (to a small extent) and enables a better understanding of this very different world.
Now, imagine being hard of hearing in a hospital
Hospitals are noisy spaces. There are alarms, ringing phones, televisions, staff, visitor, and patient conversations [3]. The Journal of the American Geriatrics Society describe hospitals as noisy, disorganized environments that make it hard for people with hearing loss, which is very common with older patients, to understand what is said [4]. A nationally representative study done in New York included 4,436 participants that were 65 years or older, all living in the community, and everyone had been checked in to the hospital at least once between 2010 and 2013. 12 % of these respondents said that they had trouble communicating because of their hearing difficulties. It also showed that hard-of-hearing patients who cannot communicate with their doctors without any problems are more likely to be reintroduced to the hospital within one month. Healthcare providers are particularly concerned about readmission because it increases the costs of the healthcare system. The report also states: ‘Trouble communicating was also associated with more health problems and worse self-rated health [4].’
Trouble communicating was associated with more health problems and worse self-rated health.
David A. Ebert, an intern in Chicago who has worked with deaf patients for many years says: 'Everybody that's involved in the field can probably tell stories about patients who were not offered adequate communication access (…), and lack of adequate communication can have dangerous implications [5].'
So, what can we do about it?
We need to better understand what is it like to be a patient with hearing loss. To do this, talk to people with hearing loss who have already come into the hospital and find out what the experience was like for them. Your current patients and staff are already a fount of knowledge and will be able to help.
interview your patients
Discover what is happening for your patients in a systematic way. This is usefully done by seeing a patients’ experience with the hospital as a map, which they travel through in a (mostly) linear way from start to finish. You should understand what was happening when the patient became aware of their need and then aware of the hospital (online or through other research), then whether an appointment was scheduled, and how they arrived. Perhaps it was an emergency. During the hospital visit, the patient might travel within the institution and then register at the reception. After waiting in the waiting area, the consult itself will normally take place. If any payments or follow ups are needed, the patient may have to go back to the reception. Before the patient leaves the hospital complex, they may also have to pay for parking. After the visit, there are possible schedules and follow-ups. They may also talk about the experience to others. All of these are important steps to discover more about.
Be specific. Ask questions like, “Remember back when you needed to get in touch with us to book an appointment, how was that for you? What were you doing, thinking and feeling?” Problems will become very clear during those interviews. You will also learn about the major touch-points (these might include your website, reception, the clinician, the parking attendant) they have with the hospital, and people who influence their perceptions of the hospital (these may be family, staff, or people in the waiting room)[6].
There are many touch-points when a person with hearing loss might have problems. It seems easy to call and make an appointment, but patients with a hearing disability cannot phone a physicians: they may have to go to the healthcare facility in person [7]. Arriving in the hospital, it may be hard understanding the voice on the intercom speaker. Being in the facility and speaking with the receptionist is the next challenge. It will get even more difficult to hear announcements in the boisterous waiting area. Patients will not hear shouted instructions or staff calling out their name. Important medical information like discussions about diagnosis and treatment options, financial obligations for services, and home care instructions will be a further challenge, with risks of being misunderstood.
Create a patient journey map
Next, summarise what you learned in a Patient Journey Map. The Patient Journey Map should be created in a way that helps everyone understand the step by step process that patients go through when they undergo treatment. There will be different maps for treatment areas. Describe all of the stages, from awareness through to referral. The Journey Map will become an important tool to communicate what is happening for a person with hearing loss to your teams, and will help facilitate any necessary changes to processes. Some problems (or, in CX language, pain points) will be easy to address. Others might require more substantial thought and potentially offer an opportunity to innovate. Solve the easy things first. We’ve shared a range of ideas in the following section. Then consider how innovating the experience [6] might help the hospital achieve better patient outcomes and lessen costs to the healthcare system.
Attending to hearing loss is a strategy that hospitals have not tried, and if they tried it, they might be able to reduce the risk of readmission for significant portion of their patients.
A. Banerjee, American Geriatric Society, 2018 [8]
Apply some of these improvements
The University of California [9] summarized the following actions that lead to improved communication for people with hearing loss:
Face the hearing-impaired person directly, on the same level and in good light whenever possible. Position yourself so that the light is shining on the speaker's face, not in the eyes of the listener.
Do not talk from another room. Not being able to see each other when talking is a common reason people have difficulty understanding what is said.
Speak clearly, slowly, distinctly, but naturally, without shouting or exaggerating mouth movements. Shouting distorts the sound of speech and may make speech reading more difficult.
Avoid talking too rapidly or using sentences that are too complex. Slow down a little, pause between sentences or phrases, and wait to make sure you have been understood before going on.
Most hearing-impaired people have greater difficulty understanding speech when there is background noise. Try to minimize extraneous noise when talking.
Some people with hearing loss are very sensitive to loud sounds. This reduced tolerance for loud sounds is not uncommon. Avoid situations where there will be loud noises when possible.
If the hearing-impaired person has difficulty understanding a particular phrase or word, try to find a different way of saying the same thing, rather than repeating the original words over and over.
Whenever possible, provide pertinent information in writing, such as directions, schedules, work assignments, etc.
The Princess Alexandra Hospital in Brisbane, Australia offers free of charge communication kits for deaf or hard-of-hearing patients. These are offered at the hospital’s interpreter service office, or can be printed out at home before the appointment. The kit contains:
- Communication alert for staff to put on the patients beside chart or whiteboard [10]
- Important hospital words in Australian sign language
- A hearing aid/cochlear implant information brochure
- A few stickers to inform staff about the patients hearing loss (they look like the communication alert)
- A plastic zip-lock bag for holding hearing aids
- A visual pain scale to help express the patients feeling [11]
- A pen for the patient to be able to write short messages and a feedback form to let the hospital know if the kit was useful [12]
https://metrosouth.health.qld.gov.au/sites/default/files/deaf-bedside-alert.pdf
Ask questions and take action
Dr McKee, a deaf physician from the U.S. advises: 'We generally do a poor job of assuming what the patients need in terms of communication preference. Instead of assuming, the first question is, "How can we effectively communicate with you?" [13]’
Asking the right questions is an excellent first move. The next step is to take action and create solutions that help those we care about receive better health outcomes.
Authors
Ulla Schneider is an intern at CapFeather and hails from Germany. Her grandmother suffers from hearing loss so she wrote this article to raise awareness in the healthcare sector.
Sarah Daly is a Founder and Director in CapFeather, a customer strategy and innovation consulting firm.
References
[1] https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss. Accessed February 23, 2021.
[2] Clason, D. (2020, February 24). Understanding the degrees of hearing loss. Healthy Hearing. Retrieved February 20, 2021 from https://www.healthyhearing.com/report/41775-Degrees-of-hearing-loss.
[3] King's College London. (2018, November 19). Noise pollution in hospitals: A rising problem. ScienceDaily. Retrieved February 21, 2021 from www.sciencedaily.com/releases/2018/11/181119064139.html.
[4] Banerjee, A. (2018, October 25). Hearing loss patients at higher risk of hospital readmission. Journal of the American Geriatrics Society. Retrieved February 20, 2021 from https://www.reuters.com/article/us-health-hearing-loss/hearing-loss-patients-at-higher-risk-of-hospital-readmission-idUSKCN1MY30I?feedType=RSS&feedName=healthNews.
[5] Frost, M. (2019, April). Listening to patients who can’t hear: Pick up tips to treat deaf and hard-of-hearing patients. American College of Physicians. Retrieved February 20 2021, from https://acphospitalist.org/archives/2019/04/listening-to-patients-who-cant-hear.htm.
[6] Dew, R., (2018) Customer Experience Innovation: How to get a lasting market edge. Emerald Publishing
[7] Ketchell, M. (2018, November 28). Accessing healthcare is challenging for Deaf people – but the best solution isn’t ‘one-size-fits-all’. The Conversation. Retrieved February 20, 2021 from https://theconversation.com/accessing-healthcare-is-challenging-for-deaf-people-but-the-best-solution-isnt-one-size-fits-all-127734.
[8] Banerjee, A. (2018, October 25). Hearing loss patients at higher risk of hospital readmission. Journal of the American Geriatrics Society. Retrieved February ??, 2021 from https://www.reuters.com/article/us-health-hearing-loss/hearing-loss-patients-at-higher-risk-of-hospital-readmission-idUSKCN1MY30I?feedType=RSS&feedName=healthNews.
[9] University of California San Francisco. Patient Education: Communicating with People with Hearing Loss. Retrieved February 20, 2021 from https://www.ucsfhealth.org/education/communicating-with-people-with-hearing-loss.
[10] https://metrosouth.health.qld.gov.au/sites/default/files/deaf-bedside-alert.pdf
[11] https://metrosouth.health.qld.gov.au/sites/default/files/deaf-visual-pain-scale.pdf
[12] https://metrosouth.health.qld.gov.au/princess-alexandra-hospital/about-us/hospital-communication-kit
[13] https://acphospitalist.org/archives/2019/04/listening-to-patients-who-cant-hear.html